
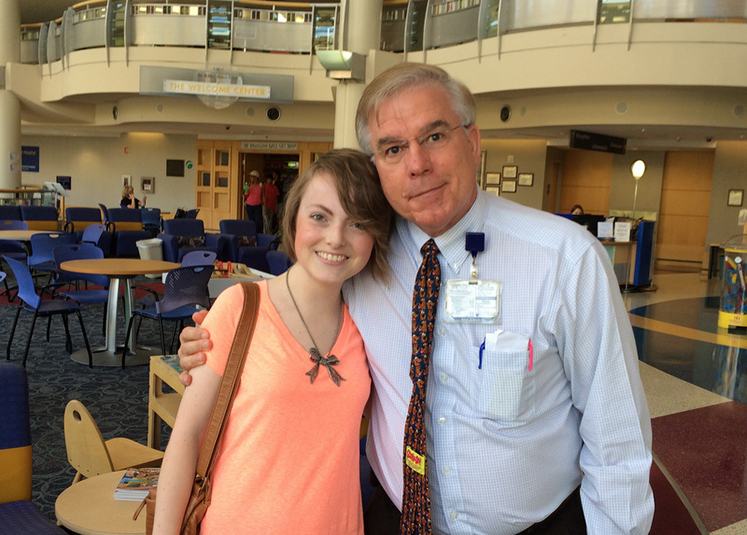
This week’s Faculty Spotlight shines on Timothy Driscoll, MD, assistant professor of pediatrics in the Division of Transplant and Cellular Therapy. Driscoll talks to us about how he became interested in medicine as early as elementary school and how he became interested in pediatric transplant and cellular therapy in particular. He also shares his reflections on the biggest current challenges and opportunities in the field and his work outside of Duke with medical missions to the impoverished people of Guayaquil, Ecuador.
How long have you been at Duke?
Since July 1, 1993.
How did you decide to come here?
Pediatric Hematology Oncology Fellowship opportunity. In addition, my brother-in-law, who is a Duke graduate, highly recommended Duke University to me.
What are your current responsibilities within the Department of Pediatrics?
Attending physician of Pediatric Transplant and Cellular Therapy Division.
Pediatric representative for Duke Pharmacy and Medication Management Committee, Duke Pharmacy and Therapeutics, 5200 Medical Director, ABMT/PBVMT/STCL Quality Assurance Program, Oncology Formulary Evaluation Team and Children’s Pharmacy and Therapeutic Chair.
Clinical oversight of cellular collection for pediatric patients for autologous stem cell transplant, Chimeric Antigen Receptor cellular therapies, dendritic cell vaccines and gene therapies.
What does your typical day look like?
This is very difficult to describe as my days are quite variable and punctuated by unpredictable events which can be very rewarding and sometimes are quite a challenge. Zoom meetings, patient care, and care coordination with Duke and outside referring physicians for time sensitive pediatric apheresis patients is rewarding and challenging. My colleagues have heard me say on multiple occasions that rarely is there a dull day on the transplant service. Unpredictable events routinely occur. For example, unplanned removal of a central line. My physician colleagues, including the PTCT nurse coordinators, PTCT nurse practitioners, PTCT office staff, 5200 PTCT nursing staff, 5200/VDH nurse manager and the CHC nursing staff, make a “typical” day a successful day.
How and when did you initially become interested in medicine?
Since elementary school! I was very close to my paternal grandfather, and I found out after I had graduated from medical school that he had wanted to be a medical doctor but that he never had the opportunity because of the Great Depression.
What made you decide to pursue a career in pediatric transplant and cellular therapy in particular?
The first cancer patient that I cared for as a pediatric resident had high risk neuroblastoma, for which high dose chemotherapy with autologous peripheral blood stem cell transplant was a standard of care. My involvement with the transplant process introduced me into the world of transplant and cellular therapy which has continued to intrigue and stimulate my scientific interests.
What do you see as the biggest current challenges and opportunities in the field of pediatric transplant and cellular therapy?
Current challenges in pediatric transplant and cellular therapy are quite numerous: host immunity and tumor interaction, reduced toxicity and increased efficacy of allogeneic hematopoietic stem cell therapies, gene therapies for hemoglobinopathies and metabolic diseases and of course application of cellular therapies to solid tumors, such as neuroblastoma.
Is there any research or other special projects you are doing or plan on doing?
Anti-CD19 Chimeric Antigen Receptor T-cell therapy for relapsed and refractory CD19(+) leukemia and Investigational Upfront Anti-CD19 Chimeric Antigen Receptor T-cell therapy for patients with NCI High Risk Leukemia: This study is exciting as it brings FDA-approved therapy for relapsed/refractory B-ALL upfront into the treatment of CD19(+) B-cell ALL which might obivate the need for a year or more of therapy. Future project of great interest is to improve survival of high risk or relapsed neuroblastoma patients by the infusion of KIR-mismatched allogeneic NK cells following completion of HSCT with standard immunotherapy.
What do you enjoy most about your work?
Improving the lives of the children/young adults who are under my care. The investment of myself into the lives of my patients is the most fulfilling way to spend my gift of life. I am gratified by my interactions with the children/young adults and their parents while providing the best available treatments, whether standard of care or experimental. I specifically chose a pediatric Heme-Onc fellowship instead of an adult fellowship because I knew the return on my personal investment would be great. A child cured of cancer would derive benefit for a lifetime.
You completed your fellowship at Duke--do you have any advice for trainees?
To be successful and fulfilled, one MUST determine one’s interests/passion to which one can devote oneself and then choose a career path that is in alignment. Life’s paths are obstructed with challenges which must be surmounted, and one’s own personal dedication will aid one to succeed and complete the race.
What passions or hobbies do you have outside of Duke?
My personal time is dedicated to my family. My parents are alive, 92 years of age and have been married for over 70 years. I have 5 siblings of which I am the third. My wife, Jeannine and daughters, Summer, Julie, Jennie and son Samuel are my focus when off Duke’s campus.
As a follower of Jesus Christ, I am very active with my family of faith and their outreaches. The projects have included over a decade of medical missions to the impoverished people of Guayaquil, Ecuador. Also, I played a role in the construction of a permanent, free standing medical clinic in Guayaquil, Ecuador that is staffed by local physicians.
Related content
A Car. And Calage.
smithellaneous.com [08.19.2016]