Welcome
Welcome to the ElMallah Lab. We are part of the Division of Pulmonary and Sleep Medicine in the Department of Pediatrics in the Duke University School of Medicine.
Our laboratory focuses on the control of breathing and pulmonary mechanics in murine models of several genetic diseases. We are currently focused on ALS mouse models and the Pompe disease mouse model. We examine the impact of gene therapy and neuromodulation on respiratory insufficiency that results from neuromuscular weakness. As a clinician scientist, my goal is to bring therapy from the bench to the bedside and enhance our research at the bench through observations at the bedside.
Research
Pompe Disease
What is Pompe disease?
Pompe disease is a fatal neuromuscular disorder resulting from mutations in the gene for acid alpha-glucosidase (GAA) – an enzyme necessary to degrade lysosomal glycogen. Infants with Pompe disease suffer from respiratory insufficiency often leading to mechanical ventilation.
The only FDA approved therapy is enzyme replacement therapy (ERT) but this therapy does not cure the muscle and CNS problems that these children encounter. Children with this disease have a weak diaphragm and upper airway dysfunction and often need a tracheostomy tube. Despite ERT, they often become dependent on a ventilator for breathing because the muscles are not fully treated with ERT. In addition, because ERT does not cross the blood brain barrier, the CNS pathology is not targeted by ERT.
Unfortunately, the only FDA approved therapy for Pompe disease enzyme replacement therapy (ERT) is suboptimal because it does not cross the blood brain barrier. Therefore, many patients on enzyme replacement therapy still require mechanical ventilation. In addition, infants and children on ERT eventually develop airway weakness and malacia.
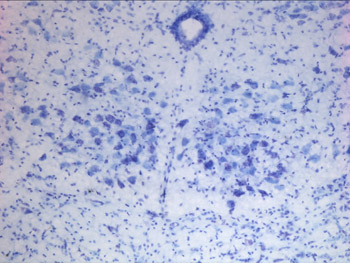
No treatment currently exists for both the CNS and muscular pathology of Pompe Disease. This research will help us better understand the mechanisms of CNS pathology involved in Pompe disease and the role of gene therapy in treating the CNS and muscular component of the upper airway problems.
Gene therapy strategy on Pompe disease
Our lab focuses on correction of the respiratory pathophysiology of Pompe disease using a Pompe disease mouse model (the Gaa-/-mouse). Using efferent nerve recordings, we are studying the impact of compounds that enhance excitatory glutaminergic neural transmission in respiratory neurons. Using rodent respiratory physiology outcome measures, such as whole body plethysmography, forced oscillometry and efferent nerve outputs we are able to study the impact of gene therapy on breathing.
Amyotrophic Lateral Sclerosis
What is Amyotrophic lateral sclerosis (ALS)?
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease with no current cure. Patients with ALS die 3-5 years after diagnosis from respiratory failure. However, if the bulbar muscles (muscles of the mouth and throat responsible for speech and swallowing) and motor neurons are affected first, death occurs within 2-3 years. Bulbar involvement results in speaking and swallowing difficulties leading to recurrent aspiration, choking and aggravation of breathing problems. The most severely affected bulbar muscle is the tongue.
In addition to tongue involvement, all individuals afflicted with ALS ultimately succumb to inadequate breathing and respiratory failure secondary to the weakness of the muscles of respiration (diaphragm and intercostal weakness). The diaphragm and intercostal muscles are essential for breathing. Initial symptoms and signs of respiratory involvement include night time carbon dioxide retention and inadequate oxygenation and ultimately decreased daytime ventilation and oxygenation. Clinically, patients present with decreased exercise tolerance, shortness of breath, early morning headaches and excessive daytime sleepiness. The rate of decline in respiratory function is related to mortality. Non-invasive ventilation with bi-level intermittent positive air pressure (BiPAP) prolongs survival significantly. The next step in respiratory support is invasive mechanical ventilation which becomes necessary for survival – however, few patients agree to the use of invasive mechanical ventilation since it places a heavy burden on their families and can lead to prolonged immobility and limited communication.
Gene therapy strategy on amyotrophic lateral sclerosis (ALS)
In collaboration with the AAV SOD1 silencing program of the Mueller lab and Brown lab, we aim to target the upper airway and phrenic motor neurons in a popular ALS mouse model – the SOD1G93A mouse with the goal of treating the respiratory insufficiency and prolonging survival.
Alpha-1 Antitrypsin Deficiency
What is Alpha-1 Antitrypsin deficiency?
Alpha-one antitrypsin (AAT) deficiency is a common (although often unrecognized) genetic disease, with up to 4% of the population carrying an abnormal AAT gene. Patients can suffer from either a lung disease, which is caused by a loss of the normal AAT action, or from a liver disease, which is caused by build-up of the abnormal mutant protein (called Z-AAT) within the liver cells.
AAT deficiency occurs worldwide, but the prevalence is variable depending on regions. It is a rare disease in Europe and in the US. It affects between 1:1500 and 1:3500 in people of European descent. It is the second most common genetic disorder in Ireland, where 1:25 people carry the mutant gene. It is rare in Asians.
Gene therapy strategy on alpha-1 antitrypsin deficiency
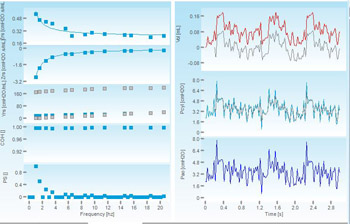
The ElMallah lab is collaborating with the Mueller lab in the characterization of the lung phenotype of Dr. Mueller’s novel alpha-1-antrypsin murine model. Specifically, we are involved in measuring the pulmonary mechanics and the awake spontaneous breathing of these novel AAT mice. These are clinically translatable measures which are comparable to respiratory findings in patients. The pulmonary mechanics we assess include measurements of respiratory compliance, resistance, elastance and other measurements. In the awake spontaneously breathing mice, we measure breathing parameters at baseline and following chemoreceptor activation. [The photo contains tracings from a FlexiVent study on Alpha-1 mice.]
Fatty Acid Oxidation Deficiencies, VLCAD
What are fatty acid oxidation deficiencies?
Fatty acid oxidation (FAO) deficiencies are a class of metabolic disorders, where the body is unable to oxidize/breakdown fatty acids to create energy because an enzyme is either missing or not working correctly. The main source of energy for the body is a sugar called glucose. Normally when the glucose runs out, fat is broken down into energy. However, that energy is not available to children and adults with these disorders. If untreated, these disorders can lead to serious complications affecting the liver, heart, eyes and general muscle development.
We focus on a family of enzymes responsible for the first step in the breakdown of fatty acid. These enzymes are known as acyl CoA dehydrogenases (ACD)’s and breakdown fatty acids of a specific length.
Very long chain acyl CoA dehydrogenases (VLCAD) deficiency is our current focus. Neonates and children with mutations resulting in complete or nearly complete loss of VLCAD may present severe hypoglycemia (can be hyperketotic), hypertrophic cardiomyopathy and sudden death.
Gene therapy strategy on fatty acid oxidation deficiencies
Using a VLCAD knockout mouse model, we aim to characterize the respiratory phenotype using whole body plethysmography, pulmonary mechanics and neurophysiology. Following this, we aim to use recombinant adeno-associated virus (rAAV) vectors as gene replacement therapy as a strategy to treat patients with these significant inherited disorders.
Lab Members

Mai ElMallah, MBBCh
Instructor in the Department of Pediatrics
Principal Investigator
Our laboratory focuses on the control of breathing and pulmonary mechanics in murine models of several genetic diseases. We are currently focuased on ALS mouse models and the Pompe disease mouse model. We examine the impact of gene therapy and neuromodulation on respiratory insufficiency that results from neuromuscular weakness. As a clinician scientist, my goal is to bring therapy from the bench to the bedside and enhance our research at the bench through observations at the bedside.

Angela McCall, PhD
Postdoctoral Associate
Angela obtained both her BS in Biochemistry & Molecular Biology and her PhD in Medical Sciences from the University of Florida. While at UF her research focused on the study of the physical properties of adeno-associated viruses and then shifted to their use as therapeutics for neuromuscular disorders. Angela’s current research goals are to connect the events that occur at the cellular level in neuromuscular disorders to the physiological changes that occur specifically those influencing respiration. She also is interested in examining how the administration of AAV-mediated gene delivery restores homeostasis at both the micro- and macroscopic levels. Outside of the lab, Angela is involved in the Hugh O’Brian Youth Leadership Organization.

Aidan Bailey
Bio coming soon.

Trey de Leon
Bio coming soon.

Justin Dhindsa
Justin is currently a senior, majoring in biology with a concentration in genomics. His research focuses on characterizing motor neuropathies in neuromuscular diseases, such as ALS, spinocerebellar ataxia type 7, and Duchenne muscular dystrophy. Justin hopes to develop and expand on his understanding of the neuropathologies underlying these diseases with exciting projects in the future. After college, he hopes to attend an MSTP program and earn his MD/PhD. Outside of the lab, Justin is involved in Duke’s chapters of Camp Kesem and Best Buddies.

Anna Fusco, BS
My name is Anna Fusco. I graduated from the University of Florida with a bachelor of science degree in biology and a minor in Italian studies. I will be attending medical school in Fall 2020. I am interested in the neural control of breathing and how respiration is impacted by neuromuscular disorders and injury in the CNS. In the lab, I focus on respiratory pathology in mice models of amyotrophic lateral sclerosis and spinocerebellar ataxia.

Logan Pucci, BS
Logan graduated from Duke University in 2020, majoring in neuroscience with minors in Spanish and chemistry. He is currently investigating the respiratory pathology of spinocerebellar ataxia type 7 (SCA7), a rare neurodegenerative disorder, in a mouse model. In the coming years, he hopes to attend medical school. Outside of the lab, Logan works as an emergency medical technician and a music producer on campus.

Laura Strickland, MS
At one point in time I wanted to become a veterinary scientist, which led me to obtain a Master of Animal Science degree at North Carolina State University. I have over four years of experience in the field of veterinary medicine as a veterinarian's assistant. In order to gain more formal research experience, I joined Dr. Mai ElMallah’s lab. My plans changed after realizing I could make more of an impact in the field of medicine by remaining at Duke University and being a part of a team that is utilizing gene therapy in order to create a better quality of life for patients and/or cure diseases. Currently, I assist with multiple projects that characterize murine models of neurodegenerative diseases, and I also lead a project that examines the effects of chronic intermittent hypoxia in an ALS mouse model. My goals are to continue moving the research in the lab forward so that we may be able to find the answers that are needed and to one day obtain my doctorate degree. When I am not doing research, I am helping with my family’s cattle farm or hiking and camping and enjoying the wonders of nature.
Publications
- Trivedi, M, ElMallah, MK, Bailey, E, Kremer, T, and Rhein, LM. "Pediatric Obstructive Sleep Apnea and Asthma: Clinical Implications (vol 46 pg e332, 2017)." PEDIATRIC ANNALS 46, no. 11 (November 2017). Full Text
- ElMallah, MK, Bailey, E, Trivedi, M, Kremer, T, and Rhein, LM. "Pediatric Obstructive Sleep Apnea in High-Risk Populations: Clinical Implications (vol 46, pg e336, 2017)." PEDIATRIC ANNALS 46, no. 11 (November 2017): E436-E436. Full Text
- Trivedi, M, ElMallah, MK, Bailey, E, Kremer, T, and Rhein, LM. "Pediatric Obstructive Sleep Apnea and Asthma: Clinical Implications." Pediatric annals 46, no. 9 (September 2017): e332-e335. Full Text
- ElMallah, MK, Bailey, E, Trivedi, M, Kremer, T, and Rhein, LM. "Pediatric Obstructive Sleep Apnea in High-Risk Populations: Clinical Implications." Pediatric annals 46, no. 9 (September 2017): e336-e339. Full Text
- Keeler, A, ElMallah, MK, and Flotte, T. "Gene Therapy 2017: Progress and Future Directions." Clinical and Translational Science 10, no. 4 (July 2017): 242-248. Full Text
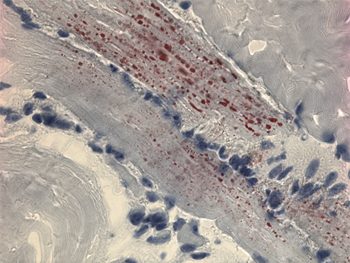
- Keeler, AM, Liu, D, Zieger, M, Xiong, L, Salemi, J, Bellvé, K, Byrne, BJ, Fuller, DD, ZhuGe, R, and ElMallah, MK. "Airway smooth muscle dysfunction in Pompe (Gaa-/- ) mice." American journal of physiology. Lung cellular and molecular physiology 312, no. 6 (June 2017): L873-L881. Full Text
- Borel, F, Sun, H, Elmallah, MK, Cox, A, Cardozo, B, Li, W, Hoffman, AM, Flotte, TR, and Mueller, C. "Editing out Five SERPINA1 Paralogs to Create a New Mouse Model of Genetic Emphysema." May 2017. Scholars@Duke
- Keeler-Klunk, AM, Zieger, M, Bircsak, S, Choudhury, S, Byrne, BJ, Sena-Esteves, M, and ElMallah, MK. "Systemic Delivery of AAVB1-GAA Gene Therapy for Respiratory Pathology in Pompe Disease." May 2017. Scholars@Duke
- Stoica, L, Keeler, AM, Xiong, L, Kalfopoulos, M, Desrochers, K, Brown, RH, Sena-Esteves, M, Flotte, TR, and ElMallah, MK. "Restrictive Lung Disease in the Cu/Zn Superoxide-Dismutase 1 G93A Amyotrophic Lateral Sclerosis Mouse Model." American journal of respiratory cell and molecular biology 56, no. 3 (March 2017): 405-408. (Letter) Full Text
- Lu, P, Liu, D, Bellve, K, Fogarty, K, ElMallah, MK, Lifshitz, L, and ZhuGe, R. "Bitter Tastant 1,10-Phenanthroline Activates Tas2r-Gustducin Signaling To Relax Airways, Resulting In A Decrease In Airway Resistance In Vivo." 2017. Scholars@Duke
- Kalfopoulos, M, Wetmore, K, and ElMallah, MK. "Pathophysiology of alpha-1 antitrypsin lung disease." In Methods in Molecular Biology, 9-19. January 1, 2017. Full Text
- Keeler, AM, Zieger, M, Liu, D, Salemi, J, ZhuGe, R, and ElMallah, MK. "Respiratory And Airway Smooth Muscle Pathology In A Pompe Disease Mouse Model." 2017. Scholars@Duke
- Turner, SM, ElMallah, MK, Hoyt, AK, Greer, JJ, and Fuller, DD. "Ampakine CX717 potentiates intermittent hypoxia-induced hypoglossal long-term facilitation." Journal of neurophysiology 116, no. 3 (September 2016): 1232-1238. Full Text
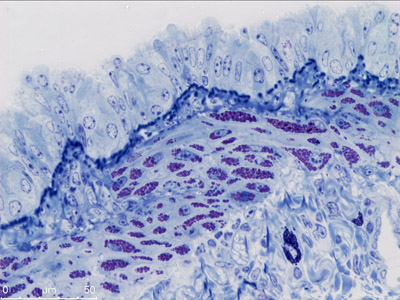
- Turner, SMF, Hoyt, AK, ElMallah, MK, Falk, DJ, Byrne, BJ, and Fuller, DD. "Neuropathology in respiratory-related motoneurons in young Pompe (Gaa(-/-)) mice." Respiratory physiology & neurobiology 227 (June 2016): 48-55. Full Text
- Borel, F, Cardozo, B, Cox, A, Li, W, Hoffman, A, ElMallah, MK, and Mueller, C. "167. Genome Editing to Generate the First Mouse Model of Alpha-One Antitrypsin Deficiency, the Leading Cause of Genetic COPD." May 2016. Full Text
- Stoica, L, Todeasa, SH, Cabrera, GT, Salameh, JS, ElMallah, MK, Mueller, C, Brown, RH, and Sena-Esteves, M. "Adeno-associated virus-delivered artificial microRNA extends survival and delays paralysis in an amyotrophic lateral sclerosis mouse model." Annals of neurology 79, no. 4 (April 2016): 687-700. Full Text
- Loring, HS, ElMallah, MK, and Flotte, TR. "Development of rAAV2-CFTR: History of the First rAAV Vector Product to be Used in Humans." Human gene therapy methods 27, no. 2 (April 2016): 49-58. (Review) Full Text
- Turner, S, Elmallah, MK, Hoyt, A, Greer, J, and Fuller, D. "Pretreatment with Ampakine CX717 Enhances Long-Term Facilitation (LTF) of Inspiratory Hypoglossal (XII) Bursting, But Only When Initial Burst Output is Low." April 2016. Scholars@Duke
- ElMallah, MK, Stanley, DA, Lee, K-Z, Turner, SMF, Streeter, KA, Baekey, DM, and Fuller, DD. "Power spectral analysis of hypoglossal nerve activity during intermittent hypoxia-induced long-term facilitation in mice." Journal of neurophysiology 115, no. 3 (March 2016): 1372-1380. Full Text
- Stoica, L, Xiong, L, Kalfopoulos, M, Desroshers, KV, and ElMallah, MK. "Characterization Of Pulmonary Mechanics Of The Sod1g93a Als Mouse Model." 2016. Scholars@Duke
- Keeler, AM, Desroshers, KV, Xiong, L, and ElMallah, MK. "Exercise Induced Respiratory Insufficiency In A Murine Model Of Very Long-Chain Acyl-Coa Dehydrogenase Deficiency." 2016. Scholars@Duke
- Borel, F, Gernoux, G, Cardozo, B, Metterville, JP, Toro Cabrera, GC, Song, L, Su, Q, Gao, GP, Elmallah, MK, Brown, RH, and Mueller, C. "Therapeutic rAAVrh10 Mediated SOD1 Silencing in Adult SOD1(G93A) Mice and Nonhuman Primates." Human gene therapy 27, no. 1 (January 2016): 19-31. Full Text
- ElMallah, MK, Pagliardini, S, Turner, SM, Cerreta, AJ, Falk, DJ, Byrne, BJ, Greer, JJ, and Fuller, DD. "Stimulation of Respiratory Motor Output and Ventilation in a Murine Model of Pompe Disease by Ampakines." American journal of respiratory cell and molecular biology 53, no. 3 (September 2015): 326-335. Full Text
- Bacewicz, A, Wang, W, Ashouri, J, and ElMallah, MK. "Children with Chronic Lung Disease: Facilitating Smoking Cessation for their Caregivers." Journal of community health 40, no. 3 (June 2015): 409-413. Full Text
- ElMallah, MK, Stanley, D, and Fuller, D. "Hypoglossal long term facilitation shifts the power spectral density to higher frequencies." April 2015. Scholars@Duke
- Turner, S, ElMallah, MK, Falk, D, Byrne, B, and Fuller, D. "Preferential Neuropathology in Respiratory-Related Motor Nuclei in Pompe Mice." April 2015. Scholars@Duke
- Falk, DJ, Todd, AG, Lee, S, Soustek, MS, ElMallah, MK, Fuller, DD, Notterpek, L, and Byrne, BJ. "Peripheral nerve and neuromuscular junction pathology in Pompe disease." Human molecular genetics 24, no. 3 (February 2015): 625-636. Full Text
- Halawa, M, Abu-Hasan, MN, and ElMallah, MK. "Hereditary mucoepithelial dysplasia and severe respiratory distress." Respiratory Medicine Case Reports 15 (2015): 27-29. Full Text
- Wang, W, Bacewicz, A, Ashouri, J, Elmallah, RK, and ElMallah, MK. "Secondhand smoke exposure in children with chronic lung disease." In Nicotine Dependence, Smoking Cessation and Effects of Secondhand Smoke, 87-121. January 1, 2015. Scholars@Duke
- Abu-Hasan, M, Elmallah, MK, Neal, D, and Brookes, J. "Salivary Amylase Level in Bronchoalveolar Fluid as a Marker of Chronic Pulmonary Aspiration in Children." Pediatric allergy, immunology, and pulmonology 27, no. 3 (September 2014): 115-119. Full Text
- Fuller, D, Elmallah, MK, Ross, H, Cerreta, A, Corti, M, Smith, B, Poirier, A, Mandel, R, and Byrne, B. "Selective knockout of acid alpha-glucosidase GAA gene expression in the medulla alters breathing." April 2014. Scholars@Duke
- Elmallah, MK, Falk, DJ, Nayak, S, Federico, RA, Sandhu, MS, Poirier, A, Byrne, BJ, and Fuller, DD. "Sustained correction of motoneuron histopathology following intramuscular delivery of AAV in pompe mice."Molecular therapy : the journal of the American Society of Gene Therapy 22, no. 4 (April 2014): 702-712. Full Text
- ElMallah, MK, Pagliardini, S, Turner, SM, Greer, JJ, Byrne, BJ, and Fuller, DD. "Ampakines Enhance Respiratory Motor Output In A Murine Model Of Pompe Disease." 2014. Scholars@Duke
- Fuller, DD, ElMallah, MK, Smith, BK, Corti, M, Lawson, LA, Falk, DJ, and Byrne, BJ. "The respiratory neuromuscular system in Pompe disease." Respiratory physiology & neurobiology 189, no. 2 (November 2013): 241-249. (Review) Full Text
- Falk, D, Todd, A, Soustek, M, Cloutier, D, ElMallah, MK, Fuller, D, and Byrne, B. "P.17.9 AAV9 vector encoding hGAA improves synaptic pathology of the neuromuscular junction in Pompe disease." October 2013. Full Text
- Falk, DJ, Mah, CS, Soustek, MS, Lee, K-Z, Elmallah, MK, Cloutier, DA, Fuller, DD, and Byrne, BJ. "Intrapleural administration of AAV9 improves neural and cardiorespiratory function in Pompe disease." Molecular therapy : the journal of the American Society of Gene Therapy 21, no. 9 (September 2013): 1661-1667. Full Text
- Sandhu, MS, Elmallah, MK, Lane, MA, Reier, PJ, Greer, JJ, and Fuller, DD. "Ampakines induce a persistent increase in phrenic motor output in rats with cervical spinal cord injury." April 2013. Scholars@Duke
- ElMallah, MK, Sandhu, MS, Lee, K-Z, Baekey, DM, and Fuller, DD. "Apnea Alters the Pattern of Intermittent Hypoxia-Induced Long Term Facilitation in Anesthetized Mice." April 2013. Scholars@Duke
- Fuller, D, Elmallah, MK, Falk, D, Lawson, LA, Martin, AD, Smith, B, and Byrne, B. "The importance of targeting the central nervous system for treatment of respiratory insufficiency in Pompe disease."February 2013. Full Text
- ElMallah, MK, and Hendeles, L. "Delivery of Medications by Metered Dose Inhaler Through a Chamber/Mask to Young Children with Asthma." Pediatric Allergy, Immunology, and Pulmonology 25, no. 4 (December 2012): 236-240. Full Text
- ElMallah, MK, Falk, DJ, Lane, MA, Conlon, TJ, Lee, K-Z, Shafi, NI, Reier, PJ, Byrne, BJ, and Fuller, DD. "Retrograde gene delivery to hypoglossal motoneurons using adeno-associated virus serotype 9."Human gene therapy methods 23, no. 2 (April 2012): 148-156. Full Text
- Elmallah, MK, Khan, Y, Hochhaus, G, Shuster, JJ, and Hendeles, L. "Systemic exposure to fluticasone MDI delivered through antistatic chambers." The Journal of allergy and clinical immunology 128, no. 5 (November 2011): 1113-5.e1-3-. (Letter) Full Text
- ElMallah, MK, Prabhakaran, S, and Chesrown, SE. "Plastic bronchitis: resolution after heart transplantation." Pediatric pulmonology 46, no. 8 (August 2011): 824-825. Full Text
- Byrne, BJ, Falk, DJ, Pacak, CA, Nayak, S, Herzog, RW, Elder, ME, Collins, SW, Conlon, TJ, Clement, N, Cleaver, BD, Cloutier, DA, Porvasnik, SL, Islam, S, Elmallah, MK, Martin, A, Smith, BK, Fuller, DD, Lawson, LA, and Mah, CS. "Pompe disease gene therapy." Human molecular genetics 20, no. R1 (April 25, 2011): R61-R68. (Review) Full Text
- Lee, K-Z, Qiu, K, Sandhu, MS, Elmallah, MK, Falk, DJ, Lane, MA, Reier, PJ, Byrne, BJ, and Fuller, DD. "Hypoglossal Neuropathology and Respiratory Activity in Pompe Mice." Frontiers in Physiology 2 (2011). Full Text
- El Mallah, MK, Sands, AJ, Casey, FA, Craig, BG, and Mulholland, HC. "Transcatheter occlusion of the patent ductus arteriosus: a comparison of two devices." Irish journal of medical science 171, no. 3 (July 2002): 151-154. Full Text
- El Mallah, MK, Chakravarthy, U, and Hart, PM. "Amblyopia: is visual loss permanent?." The British journal of ophthalmology 84, no. 9 (September 2000): 952-956. Full Text
- Chakravarthy, U, El Mallah, MK, and Hart, PM. "Amblyopia: Is visual loss permanent." March 15, 2000. Scholars@Duke